Achieving Cervical Cancer Elimination in England: Sharing Learnings, Inspiring Change
March 2025

In 2023, MSD launched the Race to Elimination campaign to showcase local areas on the road to cervical cancer elimination and inspire country-wide action. Now, taking stock of the local good practice uncovered through our ‘micro-elimination roadshow’, we’re sharing learnings to accelerate action towards elimination.
What is the opportunity?
An estimated 850 cervical cancer deaths every year – more than two women every day.[1] Nearly all cases of cervical cancer are caused by human papillomavirus (HPV), and 99.8% of cervical cancer cases are preventable through HPV vaccination, cervical screening, and early treatment of cell changes detected.[1] This provides a unique opportunity to eliminate the impact of this disease on women, their families and society.
Recognising this opportunity, in 2020, the World Health Organization (WHO) set a global strategy to work towards the elimination of cervical cancer,[2] and many individual countries have since picked up the baton in developing their own strategies for elimination. Australia, for example, is on track to be the first country to eliminate cervical cancer as soon as 2035.[3]
Where are we now?
In November 2023, NHS England joined other leading countries by making its own commitment to eliminate cervical cancer by 2040.[4] While the ambition has been set, the challenge is not insignificant and variation persists between local areas in cervical screening and HPV vaccination coverage rates.[5],[6]
Achieving cervical cancer elimination in England: sharing learnings, inspiring change
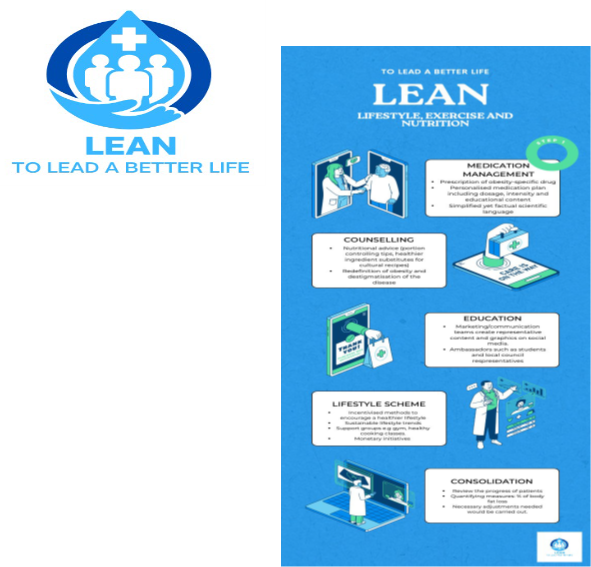
At MSD, we believe that the answers to unlocking progress in the Race to Elimination lie close to home. Local areas across the country are successfully increasing HPV vaccination and cervical screening coverage rates, and piloting new models of preventive care to improve access for underserved groups. In this context, these pockets of good practice are meeting, or even exceeding, the WHO’s thresholds, or tackling the inequalities in access experienced by some communities. In doing so, they are proof that tailored, community-focused approaches can bring us closer to hitting the WHO’s targets.
The Race to Elimination campaign has celebrated success in a number of areas across the UK – including Northumberland, Cumbria, Stockport, Liverpool and Worcestershire. Through local events held in partnership with local leaders and practitioners, we have uncovered the factors behind local progress and lessons that can be learned for the whole country.
These case studies showcase areas celebrated during the Race to Elimination, and sets out reflections on how this progress can be adapted and replicated in communities across the country.
To find out more about how we can work together to make cervical cancer elimination a reality, read our new report here.
[1] Cancer Research UK, Cervical cancer statistics. Last accessed February 2024.
[2] The World Health Organisation, Global strategy to accelerate the elimination of cervical cancer as a public health problem, November 2020. Last accessed February 2024.
[3] The Guardian, Australia on track to eliminate cervical cancer by 2035 amid rising HPV vaccination rates, February 2023. Last accessed February 2025.
[4] NHS England, NHS sets ambition to eliminate cervical cancer by 2040, November 2023. Last accessed February 2025.
[5] UK Health Security Agency, Human papillomavirus (HPV) vaccine coverage estimates in adolescents in England: academic year 2023 to 2024, January 2025. Last accessed February 2025.
[6] NHS Digital, Cervical Screening Programme, England – 2023-2024, November 2024. Last accessed February 2025.
GB-NON-11031 | February 2024